

Your Alternative to Drugs
Electrical stimulation of nerves and muscle fibers can relieve pain and activate muscle contractions without any side effects. It is a recognized method used by clinicians, doctors, physical and occupational therapists all over the world.
Several health authorities prescribe electrical stimulation for pain relief and rehabilitation and reimbursement is available from many insurance companies.
TS 6000 is a six-channel electrical stimulator designed for use in clinics and can be used with standard surface electrodes. TS 6000 is easy to use with low current and many safety features.
One waveform is often not adequate to treat all patients. But with TS 6000 you can select four different waveforms in any of the three stimulation modes: TENS, BURST, and MUSCLE.
Features
TENS mode
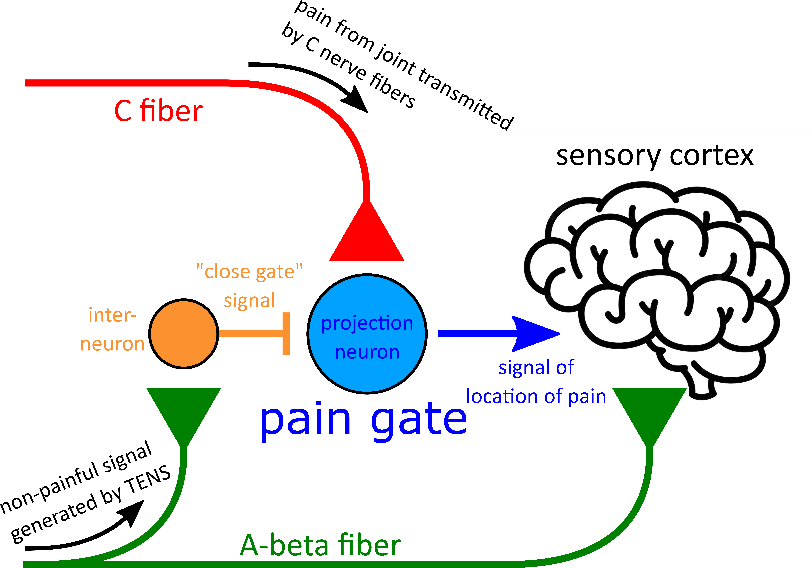
Morphine has been the main tool in pain management history, and is still popular in medical practice. But morphine can be addictive. So, doctors and scientists have been trying to find a better pain management alternative. Scientific study shows that TENS is an ideal way to achieve pain management. It sends specific low frequency pulses current through skin to the nerve to achieve the analgesic effect. When low frequency pulse current is applied to the skin, it sends stimulation via nerve pulses to the brain and pituitary, causes the release of endogenous morphine-like peptides (endorphins). The analgesia time lasts, longer. Through sending pulse current via skin to the spinal cord, it creates the effect of Gate Control (gated principal of Melzak and Wall), effectively block the pain signal to the brain, thus create pain killing analgesic effect.
BURST mode
BURST is another unique way of treating pain. BURST uses a set of high frequency, short duration periodic repetitions of low current.
BURST mode helps the body to create and release more endorphins (a chemical released by the body itself to alleviate pain.) This causes a longer lasting period of chronic pain relief in the whole body. A treatment lasts 45 minutes and will start to relieve pain in 20 minutes. Pain relief remains for another 4-12 hours and is often recommended as a supplement to TENS and when the exact area of pain is difficult to locate.
BURST is often used as an adjective therapy for TENS pain management treatment. It works well when the site of the pain is difficult to be pinpointed. BURST will also help the blood circulation, increase the temperature of cold hand and feet, help healing the wounds faster.
Dr. Ref Bkaada MD from Norway concludes based on his medical practice that it will helps the diabetes patients their blood circulation and elevating the body temperature of the hand and feet. The effect will last hours after the treatment.
MUSCLE mode
TS 6000 can also be used for rehabilitation of weak muscles and for strength training via MUSCLE mode. In MUSCLE mode, each pulse incorporates a stimulation phase to cause the muscle to contract and a pause phase to allow the muscle to relax.
MUSCLE treatment uses repeated short interval high frequency stimulation for treatment of short-term muscle injury or to restore muscle activity. A treatment for upper limb muscles lasts 10 minutes and for lower limb muscles lasts 20 minutes.
MUSCLE treatment can be carried out on the nerves and muscles to stimulate the current, thereby enhancing muscle contraction, promote blood flow, improve the flexibility of the body, and improve the body's explosive power. In particular, MUSCLE can also play a role in preventing muscle spasms. The treatment features are well suited to physical workers and athletes.
MUSCLE is commonly used in clinical rehabilitation. Stimulation of the nerves and muscles can enhance muscle contraction, promote blood circulation, improve body flexibility, prevent muscle cramps. Electrical stimulation of muscle after surgery has been widely recognized as an effective way to enhance muscle growth and speed up recovery.
Auditory-Evoked Potential for monitoring depth of anesthesia
A-line is one of the most advanced instrument for monitoring the patient’s stages of anesthesia. Using Danmeter patented technology, it monitors the existence of patients' hearing, monitors patients brain wave signals, and measures awareness level to determine the patient’s anesthesia stage to help doctors improve the accuracy of anesthesia dosage.
It helps to avoid following mistakes:

The device proactively indicates the amount of anesthesia needed for the patient based on the individual patient's consciousness through the duration of surgery.
A-line uses EEG in addition to AEP signal processing, utilizing the best of both worlds of EEG and AEP to reach perfect awareness monitoring. In processing, the A-line will show both electric signal waves of AEP and EEG.
A-line uses AAI composite index to monitor the stages and depth of anesthesia even with rapidly changing noise to signal ratio. AAI composite index retains its own characters when it is added to EEG. A-line will still be able to process the EEG signal even if patient has hearing loss. It will convert to dual frequency model when monitoring stages of anesthesia. When calculating AAI, AEP takes priority as it is the best indication for patient's awareness, as hearing is the last function the human body will lose and the first function human body will regain.
A-Line is the world's most accurate depth of anesthesia monitor.
At present, the monitoring of the depth of anesthesia is mainly based on the data of brain waves to make judgments. Brain waves are divided into spontaneous EEG (Electroencephalography) and evoked potential (EP). As the first step in the study of EEG(Electroencephalography), EEG in the removal of artifacts and EP signal extraction is particularly important.
Before talking about product A-Line, first look at several concepts: EEG, EP, AEP, ARX, AAI, A-Line.
EEG
EEG is a measurement of electrical signals of brain activity. Brain waves are the electrophysiology of brain nerve cell activity, in other words, electrical impulses in the brain. EEG is a non-invasive method that records the macroscopic electrical activity of the surface layer of the brain and cerebral cortex under the scalp with electrodes placed along the scalp. Neurons in the human brain produce ionic currents which are measured as voltage fluctuations in the EEG as seen on the right.
BIS
BIS is a statistically-based, empirically-derived complex parameter used to monitor depth of anesthesia. The bispectral index is one of several technologies used to determine the depth of anesthesia. The BIS is a weighted sum of several electroencephalographic subparameters, involving a time domain, frequency domain, and higher order spectral subparameters. A frequency spectrum and a power spectrum are derived from these EEG subparameters. In order to judge the depth of anesthesia, data are fitted with both a linear part in frequency and power to a nonlinear part with phase and harmonic information.EP
EP is the electrical response of the brain to a sensory stimulus. An evoked potential is a nervous system response signal which comprises electrical signals recorded from a specific region of the nervous system, usually measured from the cerebral cortex, brain stem, spinal cord, peripheral nerves and muscles. Evoked potential is distinct from spontaneous potentials like an EEG or other electrophysiological signals because the EP is a response elicited by a stimulus to a sensory organ, for example, an auditory click or a frequency tone stimulus presented through earphones or a flash of light on a monitor. An evoked potential or an evoked response (ER) are electrical signal responses recorded from and the stimulation of central nervous system structures, in this case, a localized area of the cerebral cortex. Evoked potentials are classified by the type of stimulus: auditory (AEP-Auditory Evoked Potentials) from acoustic stimuli, visual (VEP-Visual Evoked Potential) from light stimuli, or somatosensory (SEP-Somatosensory Evoked Potential) from tactile stimuli. It is well known in medical literature and clinical studies that hearing is the last sensation a person experiences and the first sense to recover during anesthesia and surgical operations. This makes auditory evoked potentials the more accurate and sensitive of evoked potentials.
AEP
AEPs are an electrical manifestation of the brain response to an auditory stimulus. The AEP waveform represents the passage of electrical activity provoked by auditory stimuli from the cochlea to the auditory cortex. The waves that are generated mainly in the brainstem are called brainstem auditory evoked potentials (BAEPs). The middle latency auditory evoked potentials (MLAEP) are generated from the medial geniculate and primary auditory cortex. The AEP is a weak signal (about 0.1𝜇V) masked by signals from the electroencephalogram, especially the MLAEP, which is the most suitable for detecting the depth of anesthesia and is dose-dependent as with most anesthetics. Changes can be detected on a scale normalized from 0 to 100 (from the controlled unconsciousness of general anesthesia to the emergence of a fully conscious awake state), which is by far the most accurate in the world. However, this signal is extremely weak, only 1/40 of the EEG signal strength. Extracting such a weak signal requires very advanced processing technology. The traditional moving time average (MTA) method takes about 2 minutes to process the signal, and the result is also susceptible to interference, while the autoregressive model with exogenous input (ARX model) method is used to extract the signal, and it only takes 2-6 seconds to obtain the result.
ARX
The ARX model is an advanced signal processing technique enabling 10x faster extraction of AEP index. The autoregressive model with exogenous input uses an algorithm implementing an external input automated regression mode. The use of this technology in A-Line/AEP is patented by Danmeter-Canada products.
AAI
The AAI is an ARX-extracted AEP-index which changes significantly faster than the MTA-extracted AEP. AAI stands for the AEP ARX Index. The AAI is used to monitor the depth of anesthesia of the patient by employing the principle of AEP while enabling the ARX model method of signal processing in order to extract the patient's AEP and EEG signal index.
A-Line
A-Line is one of the most advanced anesthesia depth monitoring instruments in the world. It is used in hospital wards such as operating rooms or intensive care units to monitor the depth of anesthesia and the alertness of patients during operation. Danmeter-Canada’s patented technology is able to actively test the patient’s hearing as well as brainwave activity in order to recognize the patient’s consciousness. This allows quantitative monitoring of the patient’s depth of anesthesia in real time and gives medical staff the chance to accurately control the administered amount of anesthesia.
As a consequence, following scenarios can be avoided more effectively:
A-line adds EEG in AEP signal processing, utilizing the best of the both world of EEG and AEP to reach perfect level of AAI index awareness monitoring. When in processing, A-line will show both electric signal wave of AEP and EEG.
Using AAI composite index to monitor the stages and depth of anesthesia to avoid "No Index " under rapid changing noise to signal ratio.
AAI composite index retains its own characters when it is added to EEG. A-line will still be able to process EEG signal even if patient has hearing loss. It will convert to dual frequency model when monitoring stages of anesthesia.
When calculating AAI, AEP takes priority as it is the best indication for patient 's awareness, as hearing is the last function human body will lose and the first function human body will regain.
Advantage when comparing A-Line with other similar product
There are two most commonly clinical used instruments to monitor stages of anesthesia.
It is based on two different concepts and Algorithms.
BIS and AEP:
Before we do the comparison, let's discuss the concept of BS (Burst suppression). BS is a form of brain wave, BS most often occurs during deep anesthesia. If BS constantly occurs during anesthesia, EEG is shown as equal potential, that is, a straight line shown no change in brain wave. High frequency of occurrence of BS will cause brain damage, coma, if not improved, will lead to brain death.
Now let's make a comparison between BIS and A -line:
Bispectral Index Monitoring (BIS)
BIS is the index made from measuring the linear part of EEG (including frequency and power), and nonlinear part of EEG (including phase and harmony wave ) based on EEG frequency spectrum and power spectrum . It's a mixed index by analyzing the nonlinear part of phase and harmony wave.
Following is BS index as an indicator of the stages ( depth) of anesthesia ( based on 100) :
| 100 | sober | awake |
| 100 ~ 85 | normal state | shallow anesthesia |
| 85 ~ 65 | sedative state | Moderate anesthesia |
| 65 ~ 40 | anesthesia | deep anesthesia |
| < 40 | at this time the default is likely to present the Burst Suppression | Over anesthesia |
When the index is equal or smaller than 40, BIS index can no longer shows any curve fluctuation. BS will happen often during this time. But a minority of the patients will still be awaking as the patients have not fall into deep anesthesia stage.
Auditory evoked potential difference index monitoring (AEP)
AEP is another algorithm that is different from BIS to monitor the depth of anesthesia. It is the active test of the presence or loss of hearing, combined with brainwave signals, to quantify the presence or loss of patient consciousness. AEP is more reliable, sensitive and rapid than BIS in reflecting the recovery and disappearance of consciousness, especially during anesthesia induction and recovery period.
As mentioned earlier, AAI to determine the depth of anesthesia indicators (based on 100):
| 100-60 | sober |
| 50 | Awake |
| 40 | Sedation |
| 30 | Light anesthesia |
| 20 | general anesthesia state, Surgical Anesthesia (no strong stimulation) |
| 10 | deep Anesthesia |
| < 10 | At this point the default is the possibility of burst suppression. |
Advantages of A-Line
If you take BIS to do comparison, BIS is an bispectral index to determine the stage and depth of the anesthesia. But it will not be able to provide the depth of anesthesia when the index is smaller than 40. BS could occur when the index is smaller than 40.

But AEP is able to detect the signal smaller than 40 and bigger than 10. So AEP is much more accurate in measuring the stage and depth of anesthesia.
Comparing to AEP, BIS computing speed is lot slower , showing a 30 to 60 seconds delay measuring the awareness level .
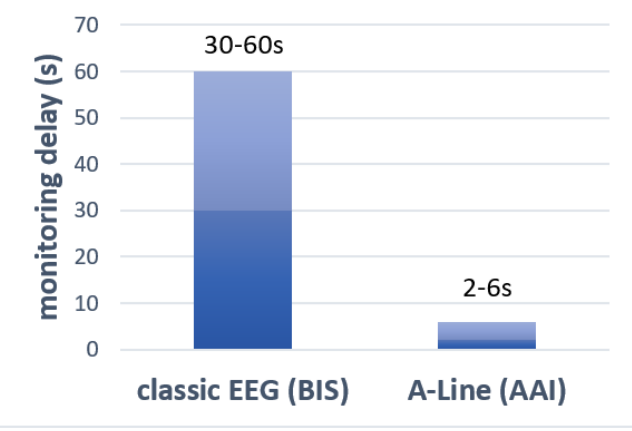
And AEP mainly used the monitoring of latency auditory evoked potential index (MLAEP) changes to determine the depth of anesthesia. The measurement speed is between 0 and 10 milliseconds. AEP is Three orders of magnitude higher than the speed of monitoring of similar products, that is, a thousand times faster.
A-line adds EEG in AEP signal processing, utilizing the best of the both world of EEG and AEP to reach perfect level of AAI index awareness monitoring. When in processing, A-line will show both electric signal wave of AEP and EEG.
AAI composite index retains its own characters when it is added to EEG. A-line will still be able to process EEG signal even if patient has hearing loss. It will convert to dual frequency model when monitoring stages of anesthesia.
AutoMove nerve stimulator for stroke recovery
The AutoMove AM800 combines the beneficial effects of both biofeedback and muscle stimulation in assisting the patient to regain a measure of control of affected limb after the occurrence of a stroke.
Using a unique "goal and reward" method the patient is gradually trained and encouraged to increase their natural strength.
This enhanced cognitive relearning process has been shown to motivate the patient to even greater performance and to significantly speed the rehabilitation process of increasing control and range of motion.
Their AutoMove AM800 is a patented instrument that helps patients with stroke (cerebral thrombosis) to rebuild and reconnect their brain nerve system network, so the paralyzed limbs can gradually regain their moving function.
Additionally, the AutoMove AM800 can treat urinary incontinence.
Most stroke patients with impaired cerebral cortical cells still have partial healthy cell left, and their cell are not 100% necrotic. AM 800 helps to train patients with cognitive relearning, and helps undamaged cell to regrow, reconnect, and to rebuild the new network. It can help the undamaged cell to reroute around the damaged brain cell to reestablish connection so to regain limb moving function.
Brain cognitive relearning and training is critical for the recovery of stroke and paralyzed patients. Undamaged nerves and cell are able to regrow and rebuild their function synapses with treatment of AM 800 instrument. Traditional physical therapy helps stroke and paralyzed patients with their muscle movement, but AM 800 helps also those patients in cognitive relearning which is critical to the recovery.

AM 800 utilize NMES to reconnect nerve cells with EMG detection. For normal person, nerve cells send out EMG that is more than 40 𝜇V in order for nerves to connect and build their network. With stroke and paralyzed patients, their nerve cells only send out EMG that is around 2 to 20 𝜇V.
AM 800 is able to detect the weakest EMG signal that stroke and paralyzed patients send. Once EMG signal pass the AM800 EMG threshold of 20 𝜇V, it activates the NMES function of AM 800 to stimulate the nerves cell, to reconnect the nerve network, so to make patients' muscle to contract and react.
AM800 also treats urinary incontinence. Using electromyography detection technology on pelvic floor, it creates a number of graphics training system for muscle movement and dual-lead EMG biofeedback treatment system. Combined with Kegel exercise, biofeedback therapy and bio electrical stimulation therapy, it is a good alternative to surgical procedure.
We formed Danmeter-Canada Enterprise Ltd. in 2009 and bought production rights for the TS 6000, AM800, and AEP from Danmeter A/S in Denmark.
Danmeter A/S was established over 20 years ago to carry out medical device research and development until its bankruptcy due to the European financial crisis.
We are seeking qualified distributors and investors.